Unit Reconstruction (Ear, Nose, Lip, Eye)
Raj D. Dedhia, MD
Assistant Professor
Division of Facial Plastic and Reconstructive Surgery
Department of Otolaryngology - Head and Neck Surgery
University of Tennessee Health Science Center, Memphis, TN, USA
Tsung-yen Hsieh, MD
Assistant Professor
Division of Facial Plastic and Reconstructive Surgery
Department of Otolaryngology - Head & Neck Surgery
University of Cincinnati
Travis T. Tollefson, MD MPH FACS
Professor
Division of Facial Plastic and Reconstructive Surgery
Department of Otolaryngology-Head and Neck Surgery,
UC Davis Medical Center
Optimal reconstruction of a given defect relies on understanding and defining the involved location and surface area, tissues layers lost, proximity to neurovascular structures, and the defect’s relationship to the facial subunits. The goals of reconstruction are to establish functional support, provide soft tissue coverage, minimize distortion, while maintaining aesthetic appearance. This module will focus on reviewing facial unit anatomy and understanding reconstruction based on aesthetic facial subunits.
- Describe the boundaries and anatomy each facial subunit.
- Review the functional and aesthetic considerations in reconstruction with respect to facial subunits.
- Describe options for reconstruction for each facial subunit based on size, structures involved, aesthetic and functional concerns.
- Recognize that there are often multiple options for reconstruction that are valid. A tailored approach based on patient factors, defect size and location, patient preference and surgeon experience is crucial to success.
- Anatomy
- Review the anatomic subunits of the nose
- Midline:
- Dorsum
- Tip
- Columella
- Paired:
- Sidewall
- Ala
- Soft-tissue triangle
- Midline:
- Review the layers of the nose
- Soft tissue envelope:
- Skin
- Subcutaneous tissue
- SMAS
- Muscle
- Bony-cartilaginous framework:
- Lower lateral cartilages
- Upper lateral cartilages
- Nasal septum
- Nasal bones
- Mucosa
- Soft tissue envelope:
- Review the anatomic subunits of the nose
- Subunits and Reconstructive Options
- Dorsum
- < 2 cm
- Round or vertically-oriented defect
- Primary closure
- “Note” flap or single transposition flap
- Bilobed flap
- Horizontally-oriented defect
- Primary closure
- Glabellar flap
- Round or vertically-oriented defect
- > 2 cm or deep defect
- Forehead flap
- < 2 cm
- Tip
- < 1.5 cm without cartilage involvement
- Primary closure
- Full thickness skin graft
- Bilobe flap
- 1.5-2.5 cm
- Superficial
- Melolabial flap
- Forehead flap
- Deep
- Forehead flap
- Superficial
- < 1.5 cm without cartilage involvement
- Columella
- Skin only
- Secondary intention
- Full thickness skin graft
- Skin and cartilage
- Good vascularity
- Composite graft
- Poor vascularity
- Melolabial flap
- Good vascularity
- Skin only
- Sidewall
- Superior aspect or medial canthal region of sidewall
- < 1 cm
- Secondary intention
- Primary closure
- Full thickness skin graft
- > 1 cm
- Secondary intention
- Glabellar flap
- < 1 cm
- Remainder of sidewall
- < 2 cm
- Bilobed flap
- Superiorly based melolabial flap
- > 2 cm
- Superiorly based melolabial flap
- Forehead flap
- < 2 cm
- Superior aspect or medial canthal region of sidewall
- Ala
- Superficial
- < 1 cm
- Overlying Alar Groove
- Secondary Intention
- Other areas
- Full thickness skin graft
- Overlying Alar Groove
- >1 cm to 2 cm
- Bilobed flap
- Melolabial flap
- < 1 cm
- Full Thickness
- < 1.5 cm
- Composite graft
- > 1.5 cm
- Melolabial turn-in flap
- Forehead flap
- < 1.5 cm
- Special Consideration: Alar rim/margin involved - consider cartilage graft to prevent retraction
- Superficial
- Soft-tissue triangle
- Mucosa-only defect with intact overlying skin-soft tissue envelope
- Composite graft
- Skin-soft tissue defect with intact mucosa
- Composite graft
- Melolabial flap with underlying cartilage graft
- Full thickness defect
- Melolabial flap with fold-in for internal lining + cartilage graft
- Forehead flap with fold-in for internal lining + cartilage graft
- Mucosa-only defect with intact overlying skin-soft tissue envelope
- Internal Lining
- Bipedicle Vestibular Skin Advancement flap
- Ipsilateral septal muchoperichondiral hinge flap
- Bilateral caudal septal muchoperichondiral hinge flap
- Contralateral dorsal septal muchoperichondiral hinge flap
- Septal composite chondromucosal flaps
- Turbinate mucoperiosteal flap
- Dorsum
References:
- Baker SR. Local Flaps in Facial Reconstruction. Philadelphia: Saunders; 2014.
- Sherris DA, Larrabee WF. Principles of Facial Reconstruction, A Subunit Approach to Cutaneous Repair. New York: Thieme; 2010.
- Constantine FC, Lee MR, Sinno S, Thornton JF. Reconstruction of the nasal soft triangle subunit. Plast Reconstr Surg. 2013;131(5):1045-50.
- Anatomy
- Review the anatomy of the auricle:
- Structures
- Helix and helical root
- Antihelix and crura
- Tragus
- Antitragus
- Lobule
- Fossae
- Scaphoid fossa
- Triangular fossa
- Concha cymba
- Concha cavum
- Structures
- Review the anatomy of the auricle:
- Subunits and reconstructive options
- Helical Rim
- Skin-only
- Full thickness skin graft
- < 1 cm
- Helical Advancement
- 2-4 cm
- Tubed postauricular pedicle flap
- Skin-only
- Antihelix
- Skin only
- Secondary intention
- Rotational advancement flap
- Full thickness skin graft
- Skin and cartilage
- < 2 cm
- Secondary intention
- Star excision
- > 2 cm or full thickness
- Composite chondrocutaneous advancement flap
- Postauricular flap with cartilage graft
- Postauricular island pedicle
- < 2 cm
- Skin only
- Combined helix and antihelical defects
- < 2 cm
- Primary closure
- Star excision
- > 2 cm
- Postauricular flap with cartilage graft
- < 2 cm
- Triangular fossa
- Partial thickness
- Secondary intention
- Full thickness skin graft
- Full thickness
- Primary closure
- Partial thickness
- Concha
- Skin only
- Secondary intention
- Full thickness skin graft
- Skin and cartilage with intact posterior skin
- Revolving door
- Full thickness
- Postauricular island pedicle
- Skin only
- Ear lobule
- Small: primary closure
- Large: postauricular flap +/- cartilage graft
- Helical Rim
References:
- Baker SR. Local Flaps in Facial Reconstruction. Saunders; 2014.
- Sherris DA, Larrabee WF. Principles of Facial Reconstruction, A Subunit Approach to Cutaneous Repair. Thieme; 2010.
- Anatomy:
- Review the anatomic subunits of the periocular area:
- upper eyelid subunit, lower eyelid subunit, lateral canthus subunit, and medial canthus subunit.
- Review the components of the lamellae of the eyelids from superficial to deep.
- Anterior lamella: skin, orbicularis oculi muscle
- Posterior lamella: tarsus, conjunctiva
- Review the anatomy of the medial canthus, lacrimal system, and lateral canthus.
- Review the anatomic subunits of the periocular area:
- Subunits and reconstructive options
- Upper eyelid subunit
- Anterior lamella only
- Primary closure
- Full thickness skin graft
- Advancement flaps
- Laterally based transposition flaps
- Full thickness
- < ¼
- primary closure
- ¼ - ½
- Primary closure with lateral cantholysis
- Tarsal rotation flap and skin muscle flap
- Tarsal rotation flap and skin graft
- ½- ¾
- Tarsoconjunctival graft and skin muscle flap
- ⅓- ⅔
- Semicircular flap with periosteal flap
- >½
- Cutler-Beard flap
- < ¼
- Anterior lamella only
- Lower eyelid subunit
- Anterior lamella only
- < 0.5cm
- Secondary intention
- > 0.5cm
- Primary closure
- Local flap
- Full thickness skin graft
- Laterally based transposition flap
- < 0.5cm
- Full thickness
- < ¼
- Primary closure
- ¼ - ½
- Primary closure with lateral cantholysis
- ½- ¾ (up to 80% with sufficient laxity)
- Tarsoconjunctival graft and skin-muscle flap
- ¼ - ⅔
- Intact lateral canthus
- Semicircular flap
- Involved lateral canthus
- Temporally based tarsoconjunctival flap
- Semicircular flap with periosteal flap
- Intact lateral canthus
- > ½
- Superiorly based tarsoconjunctival flap and skin graft
- < ¼
- Anterior lamella only
- Lateral Canthus Subunit *consider status of the lateral canthal tendon
- Secondary intention
- Primary closure
- Local flap from temple or cheek
- Medial canthus *consider status of the lacrimal system and the medial canthal tendon
- Centered or small defects
- Primary closure
- Secondary intention
- Large defects
- Delayed FTSG
- Rotational flap
- Glabellar flap
- Forehead flap
- Centered or small defects
- Upper eyelid subunit
- Lacrimal system:
- Defects in the medial eyelid or medial canthus frequently involve the lacrimal drainage system. The lacrimal system should be interrogated, and appropriate stenting and reconstruction performed if indicated.
References:
- Baker SR. Local Flaps in Facial Reconstruction. Saunders; 2014.
- Sherris DA, Larrabee WF. Principles of Facial Reconstruction, A Subunit Approach to Cutaneous Repair. Thieme; 2010.
- Anatomy
- Review the anatomic subunits of the perioral area
- Upper lip: lateral cutaneous lip subunits, phitral subunit, mucosa
- Lower lip: mucosa, cutaneous lip, mucosa, chin subunit
- Review the boundaries of the subunits: nasal base, philtral ridge, melolabial crease, vermilion borders, labiomental crease.
- Appreciate the complexity of the lip tissue and its components: skin, muscle, salivary glands, mucosa, vermillion, wet and dry lip.
- Review the anatomic subunits of the perioral area
- Lower lip partial thickness defects
- Mucosa
- Secondary intention (if small)
- Primary closure
- Local mucosal advancement flap (vermilionectomy)
- Tongue flap (Not usually first choice for reconstruction: requires 2 stages, and may be difficult for the patient while the pedicle is in place.)
- Cutaneous lip subunit
- Adjacent labiomental crease
- A to T flap
- Adjacent vermillion
- A to T flap
- Central
- Bilateral advancement
- Lateral
- Advancement, rotation, or transposition flaps
- Adjacent labiomental crease
- Chin subunit
- Adjacent labiomental crease
- A to T flap
- Midline
- Vertical primary closure
- Rotational advancement or transposition flaps
- Lateral
- Primary closure with chin advancement
- Adjacent labiomental crease
- Mucosa
- Lower lip - full thickness
- <¼ with sufficient laxity up to ⅓
- Primary closure
- ¼ - ½
- Not involving oral commissure
- Bilateral advancement flap with sufficient laxity
- Abbe flap (consider location of the philtral ridges when creating the flap)
- Involving oral commissure
- Eslander flap
- Not involving oral commissure
- ½- ⅔
- Karapandzic flap
- ⅔ - total
- Karapandzic flap
- Bernard burrow or Gillies fan flap
- Regional or free flap
- <¼ with sufficient laxity up to ⅓
- Upper Lip - partial thickness defects
- Mucosa
- Secondary intention
- Primary closure
- Local mucosal advancement
- Philtral subunit
- Secondary intention
- Full thickness skin graft
- Lateral cutaneous subunit
- 1-2 cm
- Adjacent to philtrum
- 1-2 cm
- Perialar crescentic advancement
- V-Y subcutaneous pedicle island advancement flap
- 1-2 cm
- Adjacent melolabial fold
- 1-2cm
- Primary closure
- Laterally based rotation flap
- 1-2cm
- Midportion
- 1-2cm
- Inferiorly based melolabial flap
- V-Y subcutaneous pedicle island advancement flap
- 1-2cm
- Adjacent to vermillion
- 1-2cm
- A to T flap
- 1-2cm
- Adjacent to philtrum
- >2cm
- Consider replacing the entire subunit with an inferiorly based melolabial flap.
- 1-2 cm
- Mucosa
- Upper lip - full thickness defects
- Philtral subunit not involved
- <¼
- Primary closure
- ¼ - ⅓
- Unilateral perialar crescentic advancement
- Entire lateral subunit
- Oral commissure involved
- Estlander flap
- Oral commissure not involved
- Abbe flap
- Oral commissure involved
- <¼
- Philtral subunit involved
- Philtrum only
- Primary closure
- Abbe flap for subunit
- <¾
- Perialar crescentic advancement and abbe flap
- Karapandzic flap and Abbe flap
- ⅔ - total
- Adequate cheek
- Full thickness melolabial flap and Abbe flap with mucosal advancement flap.
- Inadequate cheek
- Karapandzic and Abbe flap
- Regional flap
- Free flap
- Adequate cheek
- Philtrum only
- Philtral subunit not involved
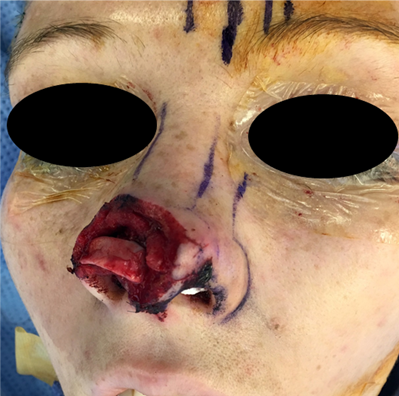
- A 20-year-old suffered a dog bite to the face resulting in a full thickness avulsion injury involving the right nasal ala, soft tissue triangle, sidewall, columella and tip (see figure below). What are your reconstruction options?

She underwent a multilayer reconstruction with bipedicled nasal mucosa graft for internal lining, alar rim graft from auricular cartilage (see intraoperative figure below), and a paramedian forehead flap.
One-year follow-up demonstrates good alar rim contour without retraction or nasal obstruction (see figure below).

- 40-year-old woman with the following defect. Please describe subunits involved and options for reconstruction.

Reconstruction performed with bilateral inferiorly based transposition melolabial flaps, mucosal advancement flap, and cheek advancement.
Intraoperative flap design and photo (the shaded area was discarded)


1 week after surgery

7 months after surgery

- What are the nasal subunits?
- List reconstruction options for a full-thickness defect of the nasal soft-tissue triangle.
- What are reconstructive options for a full-thickness defect measuring 2.5 cm involving the helix, triangular fossa and antihelix?
- What are the anatomical layers of the eyelid?
- What are the options for reconstruction of a total full thickness lower eyelid defect?
- What are options for reconstruction for a 30% full thickness defect of the lower lip involving the oral commissure? .
Learner must Sign In to access AAO-HNSF education activities.
- Annual Meeting Webcast (AMW):
- Patient Management Perspectives (Pmp):
