Orbital Neoplasms
Jason Fleming, FRCS MEd PhD
Andrew Fuson, MD
Houman Sotoudeh MD
Susan McCammon, MD
UAB, Department of Otolaryngology – Head and Neck Surgery
1155 Faculty Office Tower
510 20th Street South
Birmingham, AL 35233
Orbital tumors are a rare and diverse group of diseases. They can present with a variety of symptoms and signs, but early recognition is important. Primary orbital tumors can be benign or malignant in nature, although secondary lesions invading from local anatomical structures are more common. A variety of treatment modalities are available depending on the underlying pathology, but locally advanced disease may require an aggressive multimodality treatment plan requiring sacrifice of the orbital contents with complex reconstruction. Multidisciplinary team input is vital to optimise oncological and functional outcomes for patients.
- Review orbital and periorbital anatomy.
- Describe the more common tumor pathologies.
- Recognize the symptoms and clinical signs of an orbital neoplasm.
- Summarize the principles of management of orbital neoplasms.
- List common reconstructive options.
- Describe the bony orbital anatomy, including the component bones that create the orbit, and the anatomical relations of the orbital walls.
- Identify the name, location and contents of the orbital apertures.
- Describe the anatomical principles of the associated orbital structures: eyelids, lacrimal apparatus, extra-ocular muscles, nerves of the orbit including the optic nerve, vascular supply and orbital fat.
- Recognize the surgical spaces to help understand clinical presentation and surgical approach
- Subperiosteal
- Extraconal (peripheral)
- Intraconal (central)
- Myofascial
- Extraorbital
- Subtenons
References:
- Turvey TA, Golden BA. Orbital anatomy for the surgeon. Oral Maxillofac Surg Clin North Am. 2012; 24(4):525-536
- Kersten RC, Nerad JA. Orbital Surgery (Vol 5, Ch 86). In: Tasman W, Jaeger EA, editors. Duane’s Ophthalmology. Philadelphia: Lippincott Williams & Wilkins; 2013
- Hayek G, Mercier PH, Fournier HD. Anatomy of the Orbit and its Surgical Approach. In: Pickard JD, editor. Advanced and Technical Standards in Neurosurgery, Vol 31. Austria: Springer-Verlag; 2006
- Recognise key pathological processes and the important risk factors for the development of orbital tumors specifically, including:
- Angiogenesis
- Ultraviolet B-light exposure
- Systemic immunosuppression
- Genetics of retinoblastoma
References:
- Wackernagel W, Schoenfield L, Singh AD. Part B: Cancer Angiogenesis. In: Singh AD, Damato BE, Pe’er J, Linn Murphee A, Perry JD, editors. Clinical Ophthalmic Oncology. Philadelphia: Elsevier Saunders; 2007
- Verma V, Shen D, Sieving PC, Chan CC. The role of infectious agents in the etiology of ocular adnexal neoplasia. Surv Ophthalmol. 2008; 53(4):312-31
- Recognise that a variety of tumors can present in the orbit.
- Explain the comparative incidence of benign versus malignant disease in the pediatric and adult population.
- Identify the risk factors for a malignant orbital lesion.
- Name the most common malignancies in the pediatric (rhabdomyosarcoma) and adult populations (lymphoma).
References:
- Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: The 2002 Montgomery Lecture, part 1. Ophthalmology. 2004; 111(5):997-1008
- Hassan MW, Bakry MS, Hassan HM, Alfaar AS. Incidence of orbital, conjunctival and lacrimal gland malignant tumors in USA from Surveillance, Epidemiology and End Results, 1973-2009. Int J Ophthalmol. 2016; 9(12):1808-1813
- Explain the steps in a comprehensive evaluation and workup for the patient presenting with orbital disease.
- Appreciate symptoms suggestive of an underlying disease process including change in eye appearance, reduced acuity or diplopia, epiphora and pain/pressure.
- Describe pertinent examination findings related to position and functional assessment. This includes lid and globe position, palpation of orbital margins, lid closure, ocular motility, pupillary function, color vision, visual acuity, visual field assessment and infraorbital sensation.
- Summarize the basic principles behind more advanced ophthalmic examination techniques including testing for relative afferent pupillary defect (RAPD), exophthalmometry for proptosis and nasolacrimal system examination.
References:
- Taban M, Perry JD. Examination techniques. In: Singh AD, Damato BE, Pe’er J, Linn Murphee A, Perry JD, editors. Clinical Ophthalmic Oncology. Philadelphia: Elsevier Saunders; 2007
- Broadway DC. How to test for a relative afferent pupillary defect (RAPD). Community Eye Health. 2016; 29(96): 68–69
- Kennerdell JS, Cockerham KP, Maroon JC, Rothfys WE. Clinical evaluation. In: Kennerdell JS Cockerham KP, Maroon JC, Rothfys WE, editors. Practical diagnosis and management of orbital disease. Boston: Butterworth-Heinemann; 2001
- State that radiologic studies are essential for assessing the primary site of disease and degree of extension.
- Cite and be able to discuss the complementary information provided by computed tomography (CT) and magnetic resonance imaging (MRI) for assessing orbital disease.
- Identify of other imaging modalities available for use in specialist centres e.g. optical coherence tomography (OCT), positron emission tomography (PET).
References:
- Warner MA, Weber AL, Jakobiec FA. Benign and malignant tumors of the orbital cavity including the lacrimal gland. Neuroimaging Clin N Am. 1996;6(1):123-42.
- Héran F, Bergès O, Blustajn J, Boucenna M, Charbonneau F, Koskas P, Lafitte F, Nau E, Roux P, Sadik JC, Savatovsky J, Williams M. Tumor pathology of the orbit. Diagn Interv Imaging. 2014; 95(10):933-44.
- Classify orbital tumors into benign and malignant pathologies, which may be primary or secondary lesions. Despite a diverse array of pathologies that can present in this region, participants should take a systematic approach to site of origin and classification and be aware of the most frequent lesions together with their natural history. This should include:
- Benign lesions that may mimic malignancy (including vascular and inflammatory conditions)
- Primary malignant lesions:
- Cutaneous malignancies
- Glandular malignancies (sebaceous, lacrimal)
- Ocular
- Mesenchymal
- Lymphoproliferative
- Secondary malignant lesions
- Local invasion (skin, paranasal sinus, nasopharynx origin)
- Distant metastasis (e.g. breast, GI)
References:
- Shah JP, Patel SG, Singh B. Eyelids and Orbit (Chapter 4). In: Shah JP, Patel SG, Singh B. Jatin Shah’s Head and Neck Surgery and Oncology (4th Edition). Philadelphia: Elsevier Mosby; 2012
- Shinder R, Al-Zubidi N, Esmaeli B. Survey of orbital tumors at a comprehensive cancer center in the United States. Head Neck. 2011; 33(5):610-614
- Maheshwari A, Finger PT. Cancers of the eye. Cancer metastasis rev. 2018; 37(4):677-690
- Recognise that orbital tumors are best managed in a multi-disciplinary unit with input from a variety of teams including ophthalmology, otolaryngology, oculoplastics and oncology.
- Describe the important treatment modalities available to patients, tailored to the presenting pathology and extent of disease. These include:
- Conservative: usually for benign, stable disease where intervention would of greater risk to a functioning eye.
- Radiotherapy: used either in the primary setting (e.g. lymphoproliferative disease) or for adjuvant treatment.
- Chemotherapy/immunotherapy: often used in an adjuvant setting or in combination with other modalities. Used as first line treatment in retinoblastoma.
- Surgery, which may be conservative with eye preservation and local reconstructive techniques, or radical involving orbital exenteration +/- resection of other local structures and more complex reconstructive techniques.
References:
- Shah JP, Patel SG, Singh B. Eyelids and Orbit (Chapter 4). In: Shah JP, Patel SG, Singh B. Jatin Shah’s Head and Neck Surgery and Oncology (4th Edition). Philadelphia: Elsevier Mosby; 2012
- Quatela VC, Futran ND, Boynton JR. Eye banking: techniques for eye preservation in selected neoplasms encroaching on the globe. Otolaryngol Head Neck Surg. 1993; 108(6):662-70
- Darsaut TE, Lanzino G, Lopes MB, Newman S. An introductory overview of orbital tumors. Neurosurg Focus. 2001; 10(5):E1
- Recognize that surgery is the primary treatment modality for a significant number of orbital tumors, with a few notable exceptions (e.g. retinoblastoma, lymphoma).
- Be aware that the surgical approach must be tailored to the size and site of primary disease. Treatment options may be conservative, where possible to spare uninvolved surrounding anatomy, or radical in nature.
- Cite the indications for orbital exenteration – for treatment of locally advanced malignancy where eye-sparing techniques are inadequate, and that lid-sparing may or may not be possible.
- Explain the concept of extended exenteration with resection of the bony orbit +/- local structures
- Gain a broad understanding of reconstructive principles for surgery of the orbit
- Primary closure
- Split-thickness skin graft
- Local flap
- Regional flap
- Microvascular free flap
References:
- Perez-Morerias J, Coloma J, Prada C. Chapter 99 - Principles of orbital surgery. In: Singh AD, Damato BE, Pe’er J, Linn Murphee A, Perry JD, editors. Clinical Ophthalmic Oncology. Philadelphia: Elsevier Saunders; 2007
- Kesting MR, Koerdt S, Rommel N, Mücke T, Wolff K.-D, Nobis CP, Ringel F, Frohwitter G. Classification of orbital exenteration and reconstruction. Journal of Cranio-Maxillofacial Surgery. 2017; 45(4):467–473
- Catalano PJ, Laidlaw D, Sen C. Globe sparing orbital exenteration. Otolaryngol Head Neck Surg. 2001 Oct;125(4):379-84
- Sokoya M, Cohn J, Kohlert S, Lee T, Kadakia S, Ducic Y. Considerations in Orbital Exenteration. Semin Plast Surg. 2019 May;33(2):103-105
- Zhang Z, Ho S, Yin V, Varas G, Rajak S, Dolman PJ, McNab A, Heathcote JG, Valenzuela A. Multicentred international review of orbital exenteration and reconstruction in oculoplastic and orbit practice. Br J Ophthalmol. 2017;102(5): 654–658
- Due to diverse pathological subtypes, most orbital tumors do not fit into a staging system.
- A 73 year old retired female presented with a 12 month history of a palpable painless mass in the superolateral quadrant of the right orbit, causing gradually worsening proptosis and diplopia. Visual acuity was 30/40 bilaterally but a Hertel exopthalmometer measured 5mm of proptosis. There was no relative afferent pupillary defect but there was impaired mobility of the right eye. CT imaging revealed a well circumscribed extraconal orbital mass which demonstrated mass effect on surrounding anatomy, without any local bony erosion. An orbital biopsy through a lateral brown incision demonstrated an intermediate grade B-cell lymphoma. Radiotherapy was delivered to the involved orbit and the patient demonstrated a complete response at follow-up.
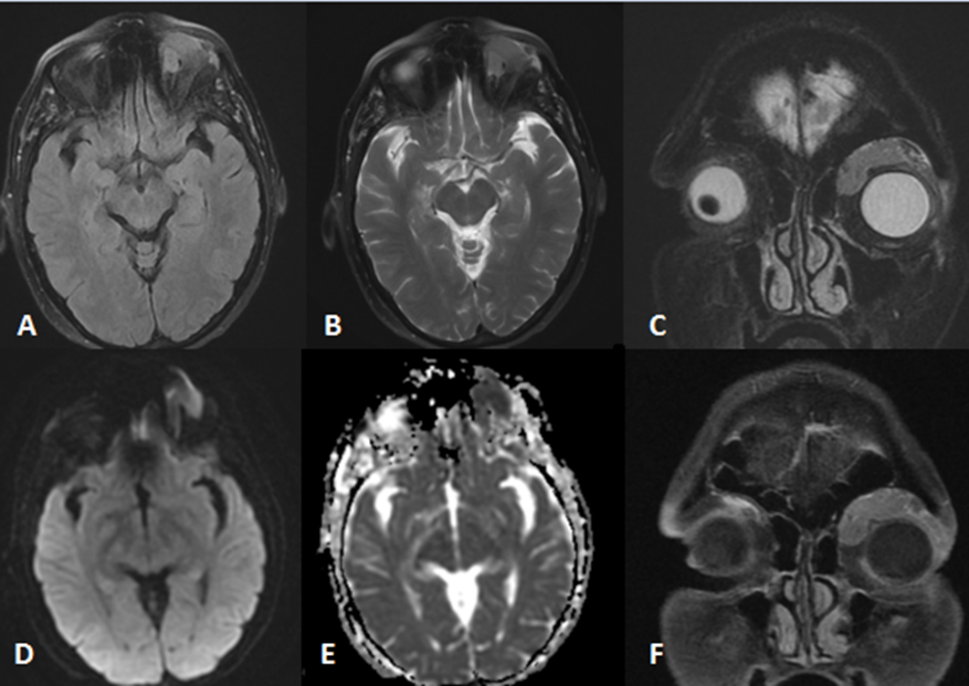
Figure 1: Axial FLAIR (A), axial T2 (B), coronal T2 (C), axial diffusion weighted sequence (D), axial ADC map (E), coronal T1 fat-sat postcontrast (F). A homogenous intraconal mass lesion located in the superior portion of the left orbit with mild mass effect over the globe. The mass lesion shows strong diffusion restriction in favor of hypercellularity. There is homogenous enhancement after contrast injection.
- A 51 year old male was referred urgently to the regional head and neck cancer unit by their optometrist with a few month’s history of a painful left eye and palpable and discharging lesion at the medial canthus. There were no complaints of diplopia, with symmetrical visual acuity of 20/25 and full range of extraocular movements, although with pain. The eyelid and globe position appeared normal, but CT and MRI imaging demonstrated a poorly defined lesion likely originating from the medial canthus region involving the medial canthal tendon, orbital fat and extending inferiorly to involve the nasolacrimal duct. Local biopsy demonstrated a poorly differentiated SCC. Following full disclosure discussion of treatment options, the patient elected to undergo an extended left orbital exenteration with medial orbitectomy/partial rhinectomy and a right radial forearm free flap reconstruction. Frozen sections from the residual nasolacrimal duct were negative and the tumor was fully resected on pathological specimen but with extensive perineural spread. Post-operative radiotherapy was delivered, and the patient remains under follow up.
- Recognise that both disease and all treatment modalities can result in both functional and cosmetic complications to the eye and periorbital region as well as a psychological burden.
- Be aware of specific complications related to:
- Disease (local invasion, distant metastases)
- Surgery (reduced acuity/loss of vision, reduced globe motility, entropion/ectropion, orbital dystopia, cosmetic alterations)
- Radiotherapy (conjunctivitis, optic atrophy, cataract, corneal/retinal damage, fistula)
References:
- Alabiad CR, Weed DT, Walker TJ, Vivero R, Hobeika GA, Hatoum GF, Shriver EM, Tse DT. En Bloc Resection of Lacrimal Sac Tumors and Simultaneous Orbital Reconstruction. Ophthalmic Plast Reconstr Surg. 2014; 30(6):459–467
- Imola MJ, Schramm VL Jr. Orbital preservation in surgical management of sinonasal malignancy. Laryngoscope. 2002; 112(8 Pt 1):1357-65
- Hoffman GR, Jefferson ND, Reid CBA, Eisenberg RL. Orbital Exenteration to Manage Infiltrative Sinonasal, Orbital Adnexal, and Cutaneous Malignancies Provides Acceptable Survival Outcomes: An Institutional Review, Literature Review, and Meta-Analysis. J Oral Maxillofac Surg. 2016; 74(3):631–643
- Gordon KB, Char DH, Sagerman RH. Late effects of radiation on the eye and ocular adnexa. Int J Radiat Oncol Biol Phys. 1995; 31(5), 1123–1139
- What are the most common types of orbital tumors presenting in a) children and b) adults?
- What factors in the patient history might suggest a malignant pathology?
- How would you investigate a patient presenting with an orbital mass?
- How could you classify the type of operation required to remove an orbital tumor?
- How would you reconstruct an orbit following an orbital exenteration?